Brief summary
Preliminary information
Influenza-A viruses (IAV) cause infections all over the world which lead to half a million fatalities each year. These influenza outbreaks occur in temperate regions during the winter months. They peak between November and March in the northern hemisphere and between May and September in the southern hemisphere. These epidemics involve the following factors: temperature fluctuations, low air humidity, too many people indoors, lack of sunlight and associated vitamin D deficiency.
Result
The detailed study by Akiko Iwasaki et al. shows once again* that excessively low humidity significantly increases susceptibility to influenza infections.
(*Lipsitch et al. 2010, 30-year study)
An excessively low humidity of 10–20% RH leads to a reduction of the self-cleaning mechanism of the respiratory tract, to a reduction of resistance against viruses and to a reduction of the functionality of the memory cells of the immune system. At a higher relative humidity (50% RH), the reduction effects do not occur.
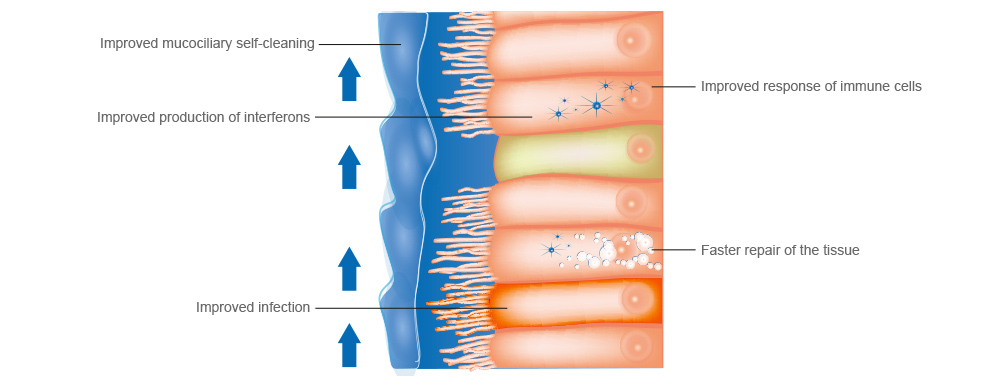
Three immune barriers to protect against infections
Protection against a viral infection should be enabled by 3 barriers of the immune system. The first barrier consists of the mucous layer, the liquid layer on the mucous layer and the
cilia on the surface. They enable the immune system to fight off pathogens and particles entering via the respiratory tract. When the virus breaks through this first immune barrier,
interferon is released to activate genes that fight and block the viruses. If the virus succeeds in penetrating this congenital second layer of defense, as the third level,
the adaptive immune system is activated in order to trigger virus-specific immune responses of the memory cells using B cells and T cells.
These three barriers become ineffective if the humidity is too low (10–20% RH). The influenza virus breaks out. The severity of the illness worsens at 10–20% relative humidity regardless of the viral burden. In addition, the ability of cellular tissue to repair itself is inhibited.
Influenza disease shows a weaker course at 50% RH with lower fever and shorter duration.
Study by Dr Akiko Iwasaki
What influences air humidity in our immune system
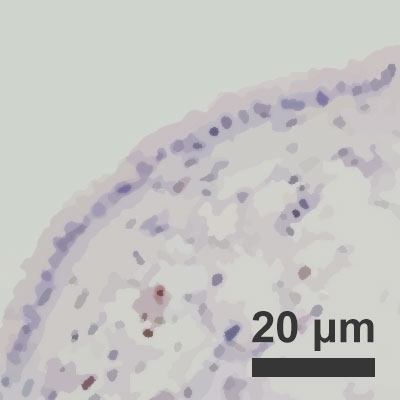
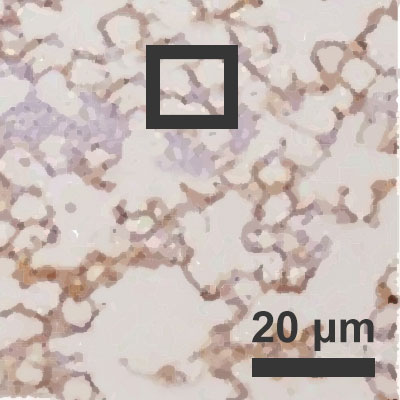 Infected pulmonary alveoli at
Infected pulmonary alveoli at 10% air humidity
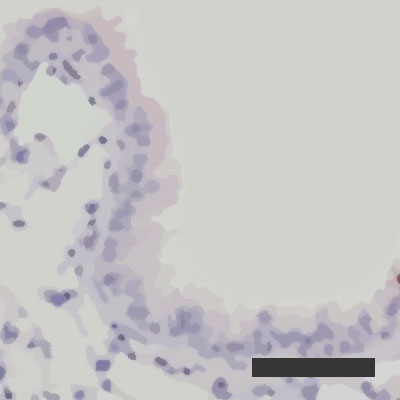
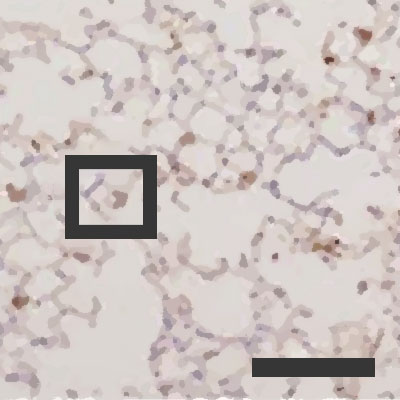 Infected pulmonary alveoli at
Infected pulmonary alveoli at 50% air humidity
 Repair activity of infected pulmonary alveoli at air humidity of 10%
Repair activity of infected pulmonary alveoli at air humidity of 10%
 Repair activity of infected pulmonary alveoli at air humidity of 50%
Repair activity of infected pulmonary alveoli at air humidity of 50%
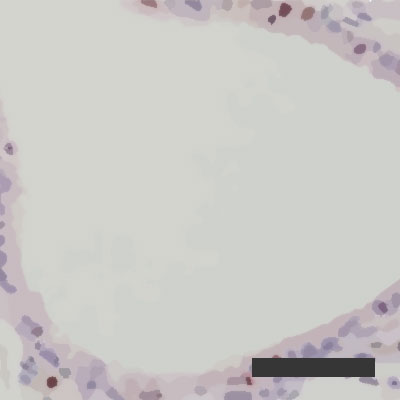 Repair activity of infected pulmonary alveoli at air humidity of 10%
Repair activity of infected pulmonary alveoli at air humidity of 10% 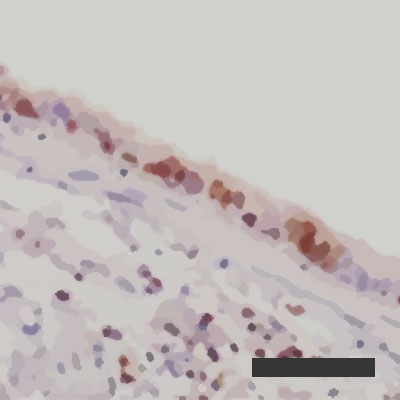 Repair activity of infected pulmonary alveoli at air humidity of 50%
Repair activity of infected pulmonary alveoli at air humidity of 50%
2 Questions for Dr. Akiko Iwasaki
How does balanced ambient air humidity affect people who are exposed to the flu virus?
What are the protective mechanisms of balanced air humidity?
We have known for decades that flu epidemics occur mainly in winter when central heating is used indoors. Possible reasons why people get sick with the flu during the winter are the subject of intense discussion. Explanations given for this seasonality include exposure to cold temperatures, low air humidity indoors or outdoors, gatherings of large groups of people in indoor areas with increased contact or droplet transmission and a reduction in the vitamin D level in healthy blood due to low exposure to sunlight.
Not only is it interesting from a theoretical viewpoint to understand the causes of the seasonal flu and therefore to know which measures can be applied in order to reduce the associated probability of illness and death. The topic is of enormous importance, as seasonal flu infections continue to increase and cause at least half a million deaths worldwide
each year. The provision of balanced air humidity is a protective measure which supports vaccination and can be used to save millions of human lives.
This study shows that dry ambient air intensifies the impacts of the flu. It was also proven that regulating the relative humidity at between 40 and 60% minimizes a viral infection and impedes the transmission process. This is the first study showing the physiological mechanisms behind the positive results that are achieved through balanced air humidity.
How does balanced ambient air humidity affect people who are exposed to the flu virus?
What are the protective mechanisms of balanced air humidity?
We have known for decades that flu epidemics occur mainly in winter when central heating is used indoors. Possible reasons why people get sick with the flu during the winter are the subject of intense discussion. Explanations given for this seasonality include exposure to cold temperatures, low air humidity indoors or outdoors, gatherings of large groups of people in indoor areas with increased contact or droplet transmission and a reduction in the vitamin D level in healthy blood due to low exposure to sunlight.
Not only is it interesting from a theoretical viewpoint to understand the causes of the seasonal flu and therefore to know which measures can be applied in order to reduce the associated probability of illness and death. The topic is of enormous importance, as seasonal flu infections continue to increase and cause at least half a million deaths worldwide
each year. The provision of balanced air humidity is a protective measure which supports vaccination and can be used to save millions of human lives.
This study shows that dry ambient air intensifies the impacts of the flu. It was also proven that regulating the relative humidity at between 40 and 60% minimizes a viral infection and impedes the transmission process. This is the first study showing the physiological mechanisms behind the positive results that are achieved through balanced air humidity.
Authors
Original title: Low ambient humidity impairs barrier function and innate resistance against influenza infection
Source link: www.pnas.org/content/early/2019/05/07/1902840116
Published: 13.05.2019
1. Wong GH, Goeddel DV (1986) Tumour necrosis factors alpha and beta inhibit virus replication and synergize with interferons. Nature 323:819–822.
2. Johnson NB, et al.; Centers for Disease Control and Prevention (CDC) (2014) CDC National Health Report: Leading causes of morbidity and mortality and associated behavioral risk and protective factors–United States, 2005-2013. MMWR Suppl 63:3–27.
3. Tamerius JD, et al. (2013) Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog 9:e1003194, and erratum 2013 Nov;9(11).
4. Alonso WJ, et al. (2015) A global map of hemispheric influenza vaccine recommendations based on local patterns of viral circulation. Sci Rep 5:1–6.
5. Tamerius J, et al. (2011) Global influenza seasonality: Reconciling patterns across temperate and tropical regions. Environ Health Perspect 119:439–445.
6. Cannell JJ, et al. (2006) Epidemic influenza and vitamin D. Epidemiol Infect 134:1129– 1140.
7. Lowen AC, Steel J (2014) Roles of humidity and temperature in shaping influenza seasonality. J Virol 88:7692–7695.
8. Eccles R (2002) An explanation for the seasonality of acute upper respiratory tract viral infections. Acta Otolaryngol 122:183–191.
9. Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M (2010) Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol 8: e1000316.
10. Lowen AC, Mubareka S, Steel J, Palese P (2007) Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog 3:1470–1476.
11. Iwasaki A, Pillai PS (2014) Innate immunity to influenza virus infection. Nat Rev Immunol 14:315–328.
12. Chen X, et al. (2018) Host immune response to influenza a virus infection. Front Immunol 9:320.
13. Garber EA, Hreniuk DL, Scheidel LM, van der Ploeg LHT (1993) Mutations in murine Mx1: Effects on localization and antiviral activity. Virology 194:715–723.
14. Staeheli P, Grob R, Meier E, Sutcliffe JG, Haller O (1988) Influenza virus-susceptible mice carry Mx genes with a large deletion or a nonsense mutation. Mol Cell Biol 8: 4518–4523.
15. Pillai PS, et al. (2016) Mx1 reveals innate pathways to antiviral resistance and lethal influenza disease. Science 352:463–466.
16. Taubenberger JK, Morens DM (2008) The pathology of influenza virus infections. Annu Rev Pathol 3:499–522.
17. Short KR, et al. (2016) Influenza virus damages the alveolar barrier by disrupting epithelial cell tight junctions. Eur Respir J 47:954–966.
18. Bustamante-Marin XM, Ostrowski LE (2017) Cilia and mucociliary clearance. Cold Spring Harb Perspect Biol 9:a028241.
19. Verhelst J, Parthoens E, Schepens B, Fiers W, Saelens X (2012) Interferon-inducible protein Mx1 inhibits influenza virus by interfering with functional viral ribonucleoprotein complex assembly. J Virol 86:13445–13455.
20. Everitt AR, et al.; GenISIS Investigators; MOSAIC Investigators (2012) IFITM3 restricts the morbidity and mortality associated with influenza. Nature 484:519–523.
21. Brass AL, et al. (2009) The IFITM proteins mediate cellular resistance to influenza A H1N1 virus, West Nile virus, and dengue virus. Cell 139:1243–1254.
22. Swiecki M, Wang Y, Gilfillan S, Lenschow DJ, Colonna M (2012) Cutting edge: Paradoxical roles of BST2/tetherin in promoting type I IFN response and viral infection. J Immunol 188:2488–2492.
23. Wang X, Hinson ER, Cresswell P (2007) The interferon-inducible protein viperin inhibits influenza virus release by perturbing lipid rafts. Cell Host Microbe 2:96–105.
24. Lenschow DJ, et al. (2007) IFN-stimulated gene 15 functions as a critical antiviral molecule against influenza, herpes, and Sindbis viruses. Proc Natl Acad Sci USA 104: 1371–1376.
25. Tang Q, Wang X, Gao G (2017) The short form of the zinc finger antiviral protein inhibits influenza A virus protein expression and is antagonized by the virus-encoded NS1. J Virol 91:e01909-16.
26. Arnheiter H, Skuntz S, Noteborn M, Chang S, Meier E (1990) Transgenic mice with intracellular immunity to influenza virus. Cell 62:51–61.
27. Kolb E, Laine E, Strehler D, Staeheli P (1992) Resistance to influenza virus infection of Mx transgenic mice expressing Mx protein under the control of two constitutive promoters. J Virol 66:1709–1716.
28. Haller O, Staeheli P, Kochs G (2007) Interferon-induced Mx proteins in antiviral host defense. Biochimie 89:812–818.
29. Allen EK, et al. (2017) SNP-mediated disruption of CTCF binding at the IFITM3 promoter is associated with risk of severe influenza in humans. Nat Med 23:975–983.
30. Randolph AG, et al.; Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network Pediatric Influenza (PICFLU) Investigators; Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network Pediatric Influenza (PICFLU) Investigators (2017) Evaluation of IFITM3 rs12252 association with severe pediatric influenza infection. J Infect Dis 216:14–21.
31. Mihaylova VT, et al. (2018) Regional differences in airway epithelial cells reveal tradeoff between defense against oxidative stress and defense against Rhinovirus. Cell Rep 24:3000–3007.e3.
32. Clary-Meinesz CF, Cosson J, Huitorel P, Blaive B (1992) Temperature effect on the ciliary beat frequency of human nasal and tracheal ciliated cells. Biol Cell 76:335–338.
33. Daviskas E, et al. (1995) Changes in mucociliary clearance during and after isocapnic hyperventilation in asthmatic and healthy subjects. Eur Respir J 8:742–751.
34. Oozawa H, et al. (2012) Effect of prehydration on nasal mucociliary clearance in low relative humidity. Auris Nasus Larynx 39:48–52.
35. Moura FE, Perdigão AC, Siqueira MM (2009) Seasonality of influenza in the tropics: A distinct pattern in northeastern Brazil. Am J Trop Med Hyg 81:180–183.
36. Shek LP, Lee BW (2003) Epidemiology and seasonality of respiratory tract virus infections in the tropics. Paediatr Respir Rev 4:105–111.
37. Horisberger MA, Staeheli P, Haller O (1983) Interferon induces a unique protein in mouse cells bearing a gene for resistance to influenza-virus. Proc Natl Acad Sci USA 80:1910–1914.
38. Grimm D, et al. (2007) Replication fitness determines high virulence of influenza A virus in mice carrying functional Mx1 resistance gene. Proc Natl Acad Sci USA 104: 6806–6811.
39. Mastorakos P, et al. (2015) Highly compacted biodegradable DNA nanoparticles capable of overcoming the mucus barrier for inhaled lung gene therapy. Proc Natl Acad Sci USA 112:8720–8725.
40. Francis R, Lo C (2013) Ex vivo method for high resolution imaging of cilia motility in rodent airway epithelia. J Vis Exp, e50343.
41. Butler A, Hoffman P, Smibert P, Papalexi E, Satija R (2018) Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat Biotechnol 36:411–420.
42. Cohen M, et al. (2018) Lung single-cell signaling interaction map reveals basophil role in macrophage imprinting. Cell 175:1031–1044.e18.
43. Steuerman Y, et al. (2018) Dissection of influenza infection In Vivo by single-cell RNA sequencing. Cell Syst 6:679–691.e4.
44. Kudo E, et al. (2019) Low ambient humidity impairs barrier function, innate resistance against influenza infection. NCBI BioProject. Available at https://www.ncbi.nlm.nih.gov/ bioproject/PRJNA528197. Deposited March 20, 2019.